After treatment for thyroid cancer, particularly following a thyroidectomy (removal of the thyroid gland), managing Thyroid-Stimulating Hormone (TSH) levels is crucial. TSH levels directly impact thyroid function, and controlling them can help reduce the risk of cancer recurrence. But what should TSH levels be after thyroid cancer, and how does the target range differ from that of people without a history of thyroid issues? This article will explore recommended TSH levels, how to monitor them, and what to expect in terms of ongoing care after thyroid cancer.
Key Takeaway:
- TSH levels are kept low after thyroid cancer to reduce recurrence risk.
- Typical target TSH: 0.1–0.5 mU/L for low-risk, below 0.1 mU/L for high-risk.
- Regular monitoring helps maintain safe suppression levels.
Table of Contents
What Should TSH Levels Be After Thyroid Cancer?
After thyroid cancer, maintaining a specific TSH level can help reduce the risk of recurrence and support overall health. Doctors typically recommend keeping TSH levels lower than average because TSH can stimulate any remaining cancerous thyroid cells.
So, what should TSH levels be after thyroid cancer? They’re often kept in a suppressed range, meaning lower than the typical TSH range for healthy individuals. This level is personalized, depending on factors like the cancer stage and the patient’s overall health.
For more details, check out here.
What Is a Normal TSH Level for Thyroid Cancer Patients?
The “normal” TSH level for thyroid cancer patients differs from the general population. In people without thyroid issues, TSH levels between 0.4 and 4.0 mU/L are generally considered normal.
For thyroid cancer patients, however, the goal is often to suppress TSH to lower-than-average levels to avoid stimulating residual cancer cells.
TSH levels between 0.1 and 0.5 mU/L are typically recommended for patients with a low to intermediate risk of recurrence, while high-risk patients may need even lower TSH levels, around 0.1 mU/L or lower.
For more details, check here.
What Should TSH Be After Thyroidectomy for Thyroid Cancer?
After a thyroidectomy for thyroid cancer, TSH levels are often intentionally kept very low. The purpose is to prevent TSH from stimulating any thyroid tissue that might remain, as this could potentially promote cancer growth.
So, what should TSH levels be after thyroid cancer and a thyroidectomy?
For many patients, a target range of 0.1 to 0.4 mU/L is common, but this is often adjusted based on individual factors and the risk of cancer recurrence. Regular monitoring and endocrinology consultations are key to keeping TSH within the desired range.
For more information, check here.
Does High TSH Mean Thyroid Cancer Recurrence?
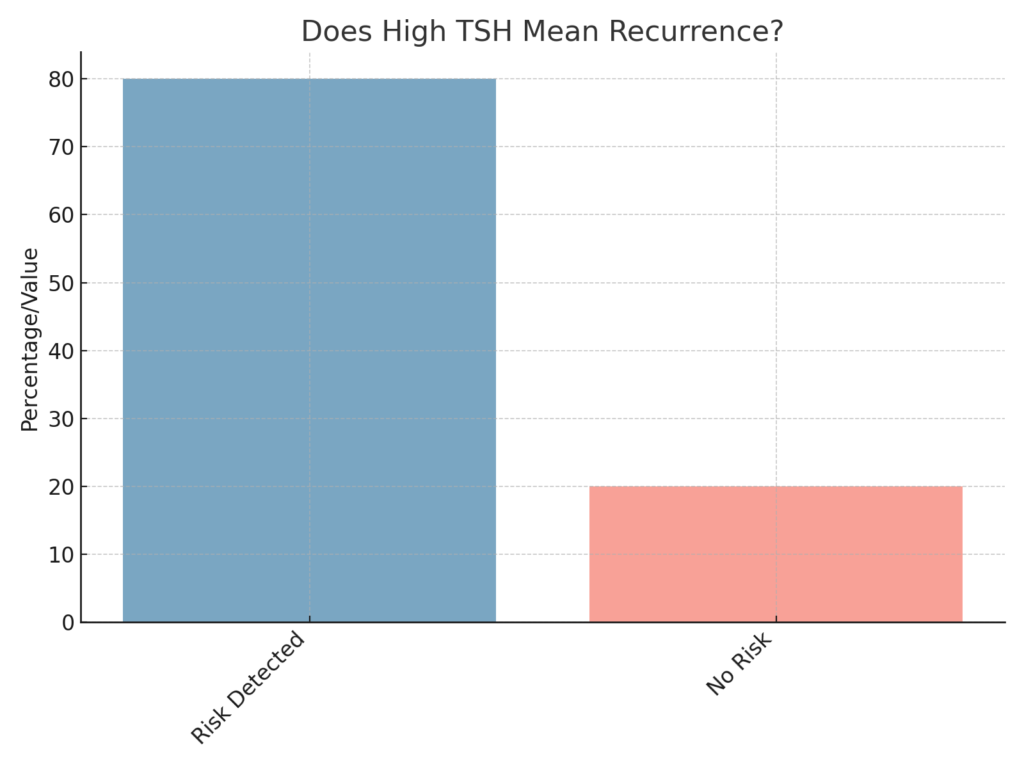
A high TSH level does not directly indicate a recurrence of thyroid cancer, but it can be a potential concern for patients who are post-treatment. Elevated TSH levels in these individuals could stimulate remaining cancerous cells if they are present.
While high TSH alone doesn’t confirm recurrence, it does prompt further testing. Doctors might use imaging or thyroglobulin tests (a marker of thyroid tissue) to investigate. Keeping TSH levels low after thyroid cancer treatment is a preventative measure to limit the chances of cancer returning.
For more details, check here.
How Suppressed Should TSH Be After Thyroid Cancer?
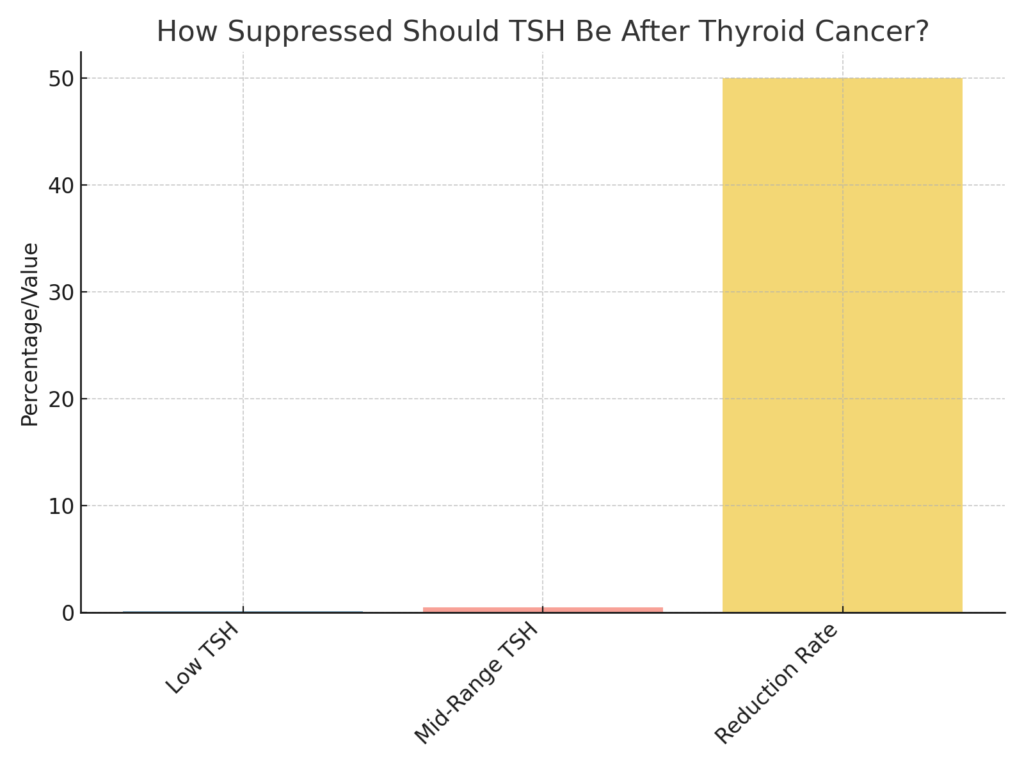
After thyroid cancer, TSH suppression is often an integral part of managing the risk of recurrence. The suppression level varies based on the cancer’s initial severity.
For patients with low recurrence risk, TSH might be maintained around 0.1 to 0.5 mU/L, while those with a higher risk could have TSH levels kept below 0.1 mU/L.
Ultimately, how suppressed TSH should be after thyroid cancer depends on factors like the cancer type, stage, and any residual thyroid tissue. This approach helps minimize the chance of stimulating any remaining cancer cells.
For more details, check here.
What Are Signs That Thyroid Cancer Has Returned?
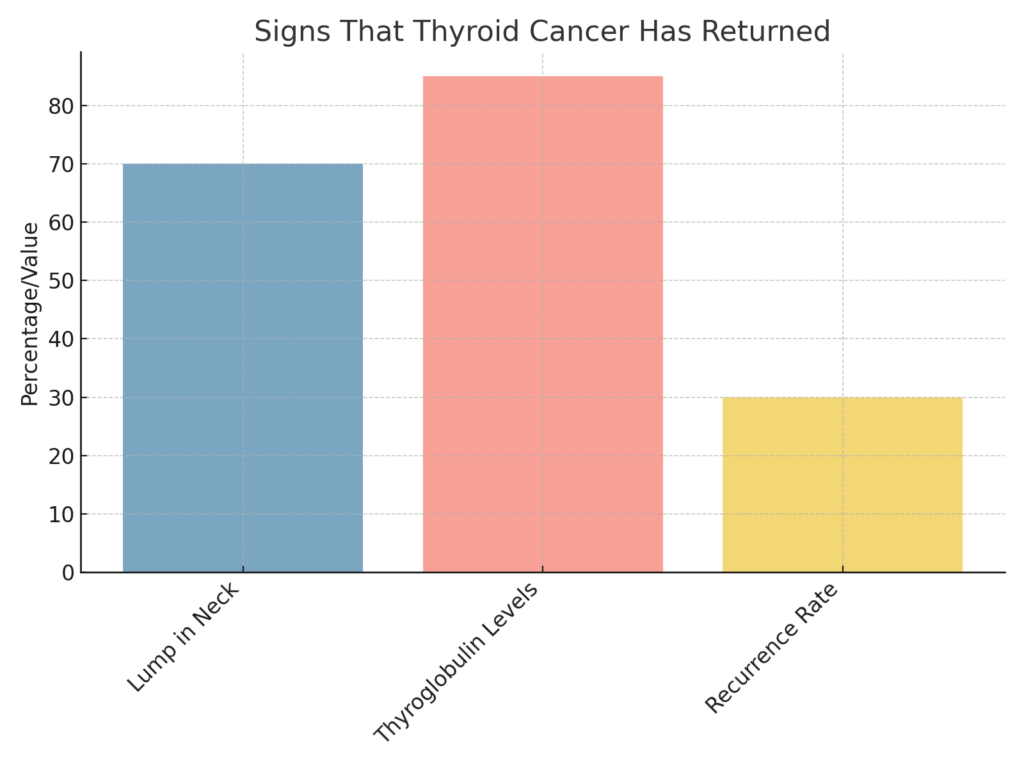
Signs of a thyroid cancer recurrence may include:
- A lump in the neck or throat area
- Difficulty swallowing or breathing
- Persistent hoarseness or voice changes
- Neck pain that doesn’t go away
- Enlarged lymph nodes
Additionally, blood tests showing elevated thyroglobulin levels can be a marker of returning thyroid tissue or cancer cells. Regular checkups and monitoring help catch any signs of recurrence early, improving the chances of successful treatment if needed.
For more information, check out here.
Does Thyroid Cancer Cause High or Low TSH?
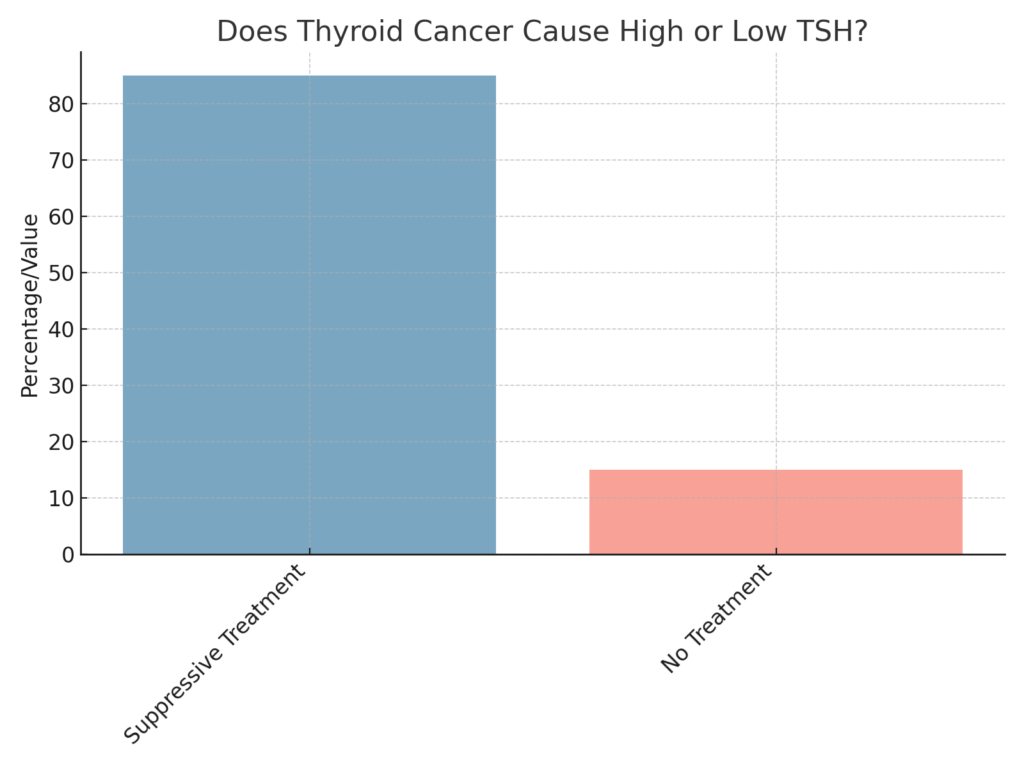
Thyroid cancer itself does not directly cause high or low TSH. TSH levels are typically more affected by thyroid function than the presence of cancer. However, doctors often manage TSH levels deliberately after thyroid cancer treatment. They might keep TSH low through hormone replacement therapy to reduce the risk of recurrence, as higher TSH levels could potentially stimulate any remaining cancerous cells.
For more information, check out here.
What Happens If Thyroid Cancer Comes Back After Thyroidectomy?
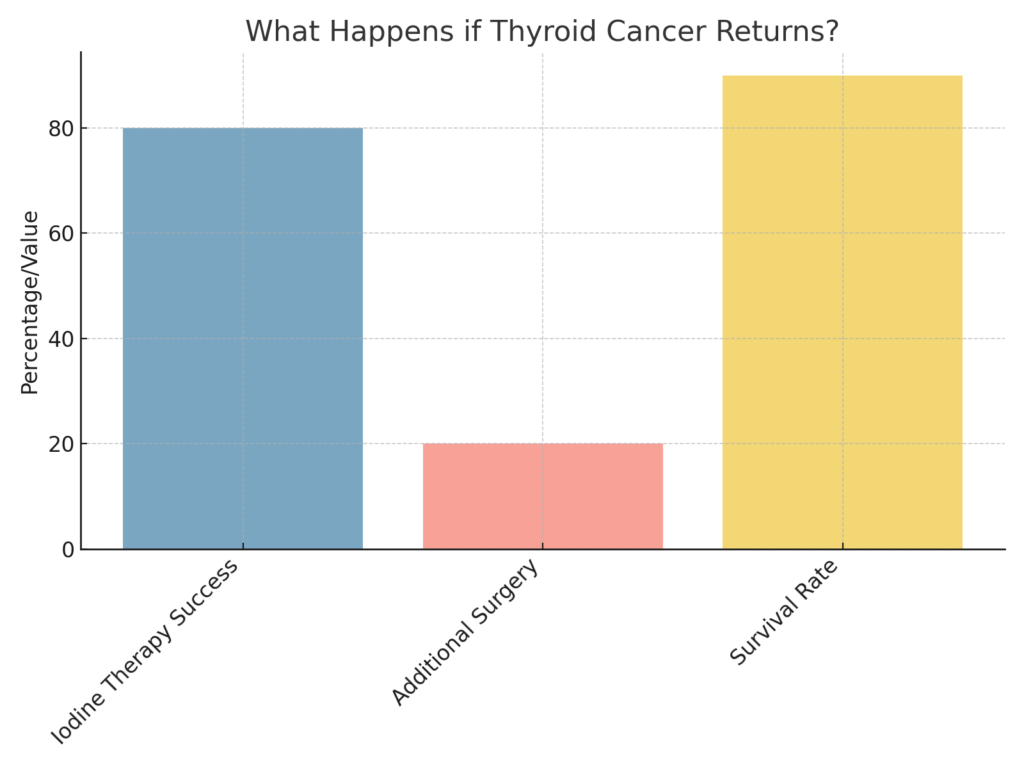
If thyroid cancer recurs after a thyroidectomy, further treatment options are available. These may include:
- Radioactive Iodine Therapy: Often used to target any remaining thyroid cells that could be cancerous.
- Surgery: In cases of a localized recurrence, surgery may be done to remove new tumor growth.
- Radiation Therapy: External beam radiation is sometimes used if the cancer cannot be removed surgically.
- Chemotherapy or Targeted Therapy: These treatments are used less frequently but may be considered for aggressive recurrences.
Follow-up care with an endocrinologist and oncologist is essential to determine the best approach for managing a recurrence.
For more details, check here.
Related:
FAQs: How Suppressed Should TSH Be After Thyroid Cancer?
After thyroid cancer treatment, TSH suppression is commonly used to reduce the risk of cancer recurrence. The degree of suppression depends on individual risk factors. Generally:
- Low-risk patients (with no signs of metastasis or aggressive cancer) might have TSH maintained between 0.1 and 0.5 mU/L.
- Intermediate- to high-risk patients (with higher chances of recurrence) are often kept at a TSH level of 0.1 mU/L or lower.
The goal is to limit any stimulation of thyroid cells, including any potentially cancerous cells that may remain. An endocrinologist will monitor TSH and adjust treatment as needed to keep levels within the safest range for each patient.
What Is a Dangerously Low Level of TSH?
A dangerously low TSH level is generally considered to be close to or below 0.1 mU/L, though this can vary based on individual health needs. Extremely low TSH levels (below 0.1 mU/L) can lead to symptoms of hyperthyroidism, such as:
- Heart palpitations and rapid heartbeat
- Anxiety or irritability
- Tremors
- Increased risk of osteoporosis, especially in older adults
While TSH suppression is often needed for thyroid cancer patients, it’s essential that it’s carefully managed to avoid these side effects. Regular follow-up testing helps ensure that TSH suppression is balanced with overall health.
Why Is My TSH Low but T3 and T4 Normal?
A low TSH with normal T3 and T4 levels may be due to subclinical hyperthyroidism or simply the result of thyroid medication adjustments. Here are some common reasons for this pattern:
- Medication Effects: In patients on thyroid hormone replacement, TSH can drop without changing T3 and T4 levels significantly. This is common when TSH is being purposefully suppressed, as in post-thyroid cancer cases.
- Subclinical Hyperthyroidism: In this condition, TSH is low, but T3 and T4 levels stay within normal limits. It may not cause noticeable symptoms, but it does require monitoring as it can impact heart health and bone density over time.
- Pituitary Gland Function: Occasionally, low TSH with normal thyroid hormone levels may indicate an issue with the pituitary gland, which controls TSH production.
Consulting an endocrinologist can help clarify the cause of this pattern and determine if adjustments in medication or further tests are needed.
Conclusion
For thyroid cancer survivors, monitoring and managing TSH levels is a key part of post-treatment care. So, what should TSH levels be after thyroid cancer? Typically, they are kept lower than average to help prevent recurrence.
By working with an endocrinologist, patients can adjust their TSH levels through medication to maintain a balance that minimizes the risk of cancer returning. With regular follow-up appointments, thyroid cancer patients can effectively manage their TSH levels and enjoy a healthy, cancer-free life.
Reference
- Grant CS. Recurrence of papillary thyroid cancer after optimized surgery. Gland Surg. 2015 Feb;4(1):52-62. doi: 10.3978/j.issn.2227-684X.2014.12.06. PMID: 25713780; PMCID: PMC4321046.
- Alaraifi AK, Alessa M, Hijazi LO, Alayed AM, Alsalem AA. TSH level as a risk factor of thyroid malignancy for nodules in euthyroid patients. Acta Otorhinolaryngol Ital. 2023 Jun;43(3):183-188. doi: 10.14639/0392-100X-N2288. PMID: 37204842; PMCID: PMC10198371.
- Li, X., Yan, L., Xiao, J., Li, Y., Zhu, Y., Yang, Z., … Luo, Y. (2023). Optimal thyrotropin level for low-risk papillary thyroid carcinoma after ultrasound-guided radiofrequency ablation. International Journal of Hyperthermia, 40(1). https://doi.org/10.1080/02656736.2022.2160880
- Mansy I, Elsenosy AM, Hassan EM, Zakria M. A Clinical Audit of Thyroid Hormonal Replacement After Total Thyroidectomy. Cureus. 2023 Dec 12;15(12):e50374. doi: 10.7759/cureus.50374. PMID: 38116025; PMCID: PMC10730255.
- Xiang Y, Xu Y, Bhandari A, Sindan N, Hirachan S, Yang Q, Guo G, Shen Y. Serum TSH levels are associated with postoperative recurrence and lymph node metastasis of papillary thyroid carcinoma. Am J Transl Res. 2021 Jun 15;13(6):6108-6116. PMID: 34306349; PMCID: PMC8290771.
- Lee YM, Jeon MJ, Kim WW, Sung TY, Chung KW, Shong YK, Hong SJ. Optimal Thyrotropin Suppression Therapy in Low-Risk Thyroid Cancer Patients after Lobectomy. J Clin Med. 2019 Aug 22;8(9):1279. doi: 10.3390/jcm8091279. PMID: 31443521; PMCID: PMC6780946.
- Xu B, Gu SY, Zhou NM, Jiang JJ. Association between thyroid stimulating hormone levels and papillary thyroid cancer risk: A meta-analysis. Open Life Sci. 2023 Aug 11;18(1):20220671. doi: 10.1515/biol-2022-0671. PMID: 37588997; PMCID: PMC10426723.
- Emilio Fiore, Paolo Vitti, Serum TSH and Risk of Papillary Thyroid Cancer in Nodular Thyroid Disease, The Journal of Clinical Endocrinology & Metabolism, Volume 97, Issue 4, 1 April 2012, Pages 1134–1145, https://doi.org/10.1210/jc.2011-2735
