TIRADS represents the Thyroid imaging reporting and data system, a classification system utilized by radiologists. It was invented in 2009 and modeled on BIRADS, the breast imaging reporting and data system of the American College of Radiology.
It’s a standardized system that classifies thyroid nodules into several levels of suspicion to check the risk of malignancy in thyroid nodules based on specific ultrasound features. This means that each nodule has a TIRADS classification that aligns with its particular malignancy risk.
The concept of TIRADS can be cost-effective and was developed to help you as an individual with thyroid nodules to avoid unnecessary FNA biopsy.
As you continue to read this article, you’ll be getting to understand the TIRADS system alongside the risks of malignancy that can be associated with it.
Key Takeaway:
Here’s a quick summary of the risks of malignancy for TIRADS:
- Thyroid Imaging Reporting and Data System (TIRADS): A classification system that categorizes thyroid nodules based on ultrasound characteristics to assess malignancy risk.
- Risk Categories: TIRADS classifies nodules from TR1 (benign) to TR5 (highly suspicious for malignancy).
- Risk Percentages:
- Diagnostic Usefulness: Helps in deciding which nodules may need biopsy, minimizing unnecessary procedures.
- Limitations: TIRADS is a guideline; clinical judgment and additional factors should still inform biopsy and treatment decisions.
- Follow-Up: Higher TIRADS levels typically require closer monitoring or further diagnostic procedures.
Table of Contents
What Are The Risk Of Malignancy For TIRADS?
Trying to get to know the TIRADS system and its associated risks of malignancy will help you as an individual (either as a patient or healthcare provider) to make logical decisions regarding further evaluation and management of thyroid nodules.
Meanwhile, the risk of malignancy in thyroid nodules is checkmated based on specific ultrasound features which include the nodule’s shape, composition, margin, echogenicity, and presence of echogenic foci.
Classification of TIRADS and its associated Malignancy Risks include:
1# TR1: Benign
The thyroid nodules in this category are known to be benign and are characterized by simple cystic or spongiform appearances and will not require further evaluation or biopsy. It comes with a malignancy risk of less than one percent.
For more information, check here.
2# TR2: Not Suspicious
The thyroid nodules in this category are characterized by the composition of colloid cysts or have other benign features on ultrasound. It’s usually not necessary to do any follow-up on the emergence of these nodules unless there are changes in the nodule’s characteristics. It comes with a very low risk of malignancy of about two percent.
For more information, check here.
3# TR3: Mildly Suspicious
The thyroid nodules in this category are characterized by the exhibition of maybe one or two suspicious features like irregular margins or hypoechogenicity. Based on a recommendation, it may become necessary to do a follow-up on the emergence of these nodules as dependent on the nodule’s size and patient factors. Follow-up can be done with an ultrasound or fine-needle aspiration (FNA) biopsy. These nodules come with a low risk of malignancy of about five percent.
For more information, check here.
4# TR4: Moderately Suspicious
The thyroid nodules in this category are characterized by their exhibition of various suspicious features like irregular margins, microcalcifications, and taller-than-wide shapes. Based on recommendation, fine-needle aspiration (FNA) biopsy is usually used in assessing the nature of the nodules and how to adequately manage them. It comes with a moderate risk of malignancy of between ten to twenty percent.
For more information, check here.
5# TR5: Highly Suspicious
The thyroid nodules in this category are characterized by their exhibition of multifold suspicious features, with a higher likelihood of becoming malignant. Based on recommendation, fine-needle aspiration (FNA) biopsy is strongly advised. In a case where malignancy is proven, removal of the thyroid nodules may be needed and done via surgery. These nodules come with a high risk of malignancy of about thirty-five percent or more.
For more information, check here.
Related:
- When to Worry About Thyroid Nodules?
- How to Shrink a Goiter Naturally
- Exercise After Radiofrequency Ablation
- Can You Live Without a Thyroid?
- What Should TSH Levels Be After Thyroid Cancer?
- How Fast Do Thyroid Nodules Grow?
- How Do I Know If My Thyroid Nodule is Benign?
- What Are the Symptoms of Cancerous Thyroid Nodules?
- Is TIRADS 3 a Treatment?
- Thyroid Ultrasound: Normal vs. Abnormal Findings
- What Foods Reduce Thyroid Nodules?
- What is a TIRADS Category 6?
What are the risk categories for ACR TIRADS?
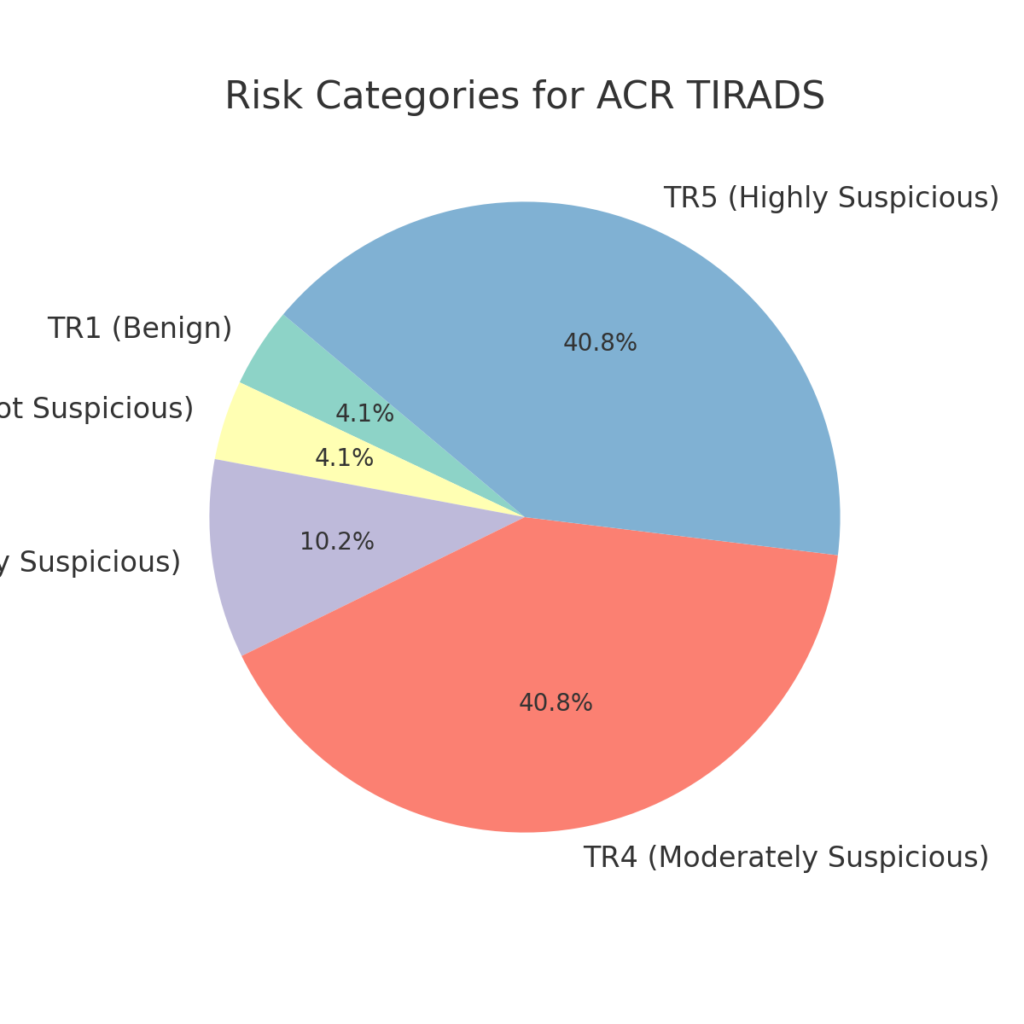
The American College of Radiology (ACR) TIRADS classifies thyroid nodules by risk level based on ultrasound characteristics:
- TR1 (Benign): 0 points — Nodules with no suspicious features; malignancy risk <2%.
- TR2 (Not suspicious): 2 points — Low-risk features; malignancy risk <2%.
- TR3 (Mildly suspicious): 3 points — May include cystic or spongiform nodules; malignancy risk 2-5%.
- TR4 (Moderately suspicious): 4-6 points — Nodules with some suspicious features; malignancy risk 5-20%.
- TR5 (Highly suspicious): 7+ points — Nodules with significant suspicious features (e.g., irregular margins); malignancy risk >20%.
What is the risk of malignancy in a hot thyroid nodule?
- Hot nodules refer to thyroid nodules that take up radioactive iodine during imaging, indicating that they are functionally active or “hyperfunctioning.”
- Risk of Malignancy: Hot nodules have a low risk of malignancy, generally <1%, as most are benign and linked to hyperthyroidism rather than cancer.
What is the risk of malignancy in thyroid nodules 4 cm or larger?

- Larger nodules (4 cm or more) tend to have a slightly higher malignancy risk.
- Malignancy Risk: Studies suggest that nodules 4 cm or larger may carry a malignancy risk between 10-15%, especially if suspicious features are present on ultrasound.
- Clinical Approach: For nodules of this size, fine-needle aspiration (FNA) or even surgical consultation is often recommended to assess risk.
What features indicate a higher risk of malignancy in the thyroid?
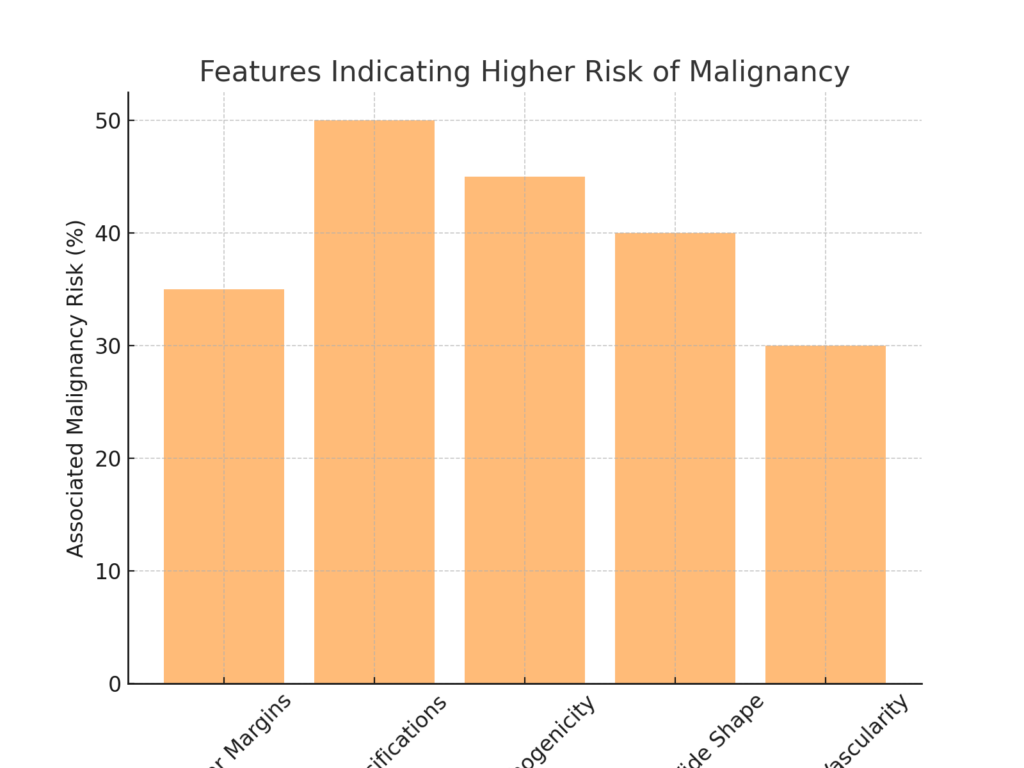
Certain ultrasound features are associated with an increased risk of malignancy in thyroid nodules:
- Irregular or Lobulated Margins: Nodules with poorly defined or irregular edges.
- Microcalcifications: Small, punctate calcifications within the nodule.
- Marked Hypoechogenicity: Nodules that appear darker than surrounding tissue on ultrasound.
- Taller-than-Wide Shape: Nodules that are taller in the vertical dimension than they are wide.
- Increased Vascularity: Nodules with more blood flow, especially in central areas.
These features are used in TIRADS scoring systems and are often considered in biopsy decisions.
Conclusion
Most thyroid nodules are accidental discoveries from simple medical routine check-ups or imaging studies, and while most may not pose any serious threat to your health as an individual, others may be malignant.
It’s seen that TIRADS 4 and 5 are highly suggestive of malignant nodules and need more diagnostic approaches plus FNA biopsy.
By classifying nodules into several levels of suspicion, TIRADS helps guide clinical decision-making and ensures that patients receive appropriate evaluation and management.
Reference
- Lin SJ, Zhang Y, Liu NC, Yang DR, Li G, Chang C. Minireview: Pathophysiological roles of the TR4 nuclear receptor: lessons learned from mice lacking TR4. Mol Endocrinol. 2014 Jun;28(6):805-21. doi: 10.1210/me.2013-1422. Epub 2014 Apr 4. PMID: 24702179; PMCID: PMC4042077.
- Venkatesh N, Ho JT. Investigating thyroid nodules. Aust Prescr. 2021 Dec;44(6):200-204. doi: 10.18773/austprescr.2021.055. Epub 2021 Dec 1. PMID: 35002033; PMCID: PMC8671014.
- Xie L, Yang R, Liu S, Lyle S, Cotsarelis G, Xiang L, Zhang L, Li B, Wan M, Xu X. TR3 is preferentially expressed by bulge epithelial stem cells in human hair follicles. Lab Invest. 2016 Jan;96(1):81-8. doi: 10.1038/labinvest.2015.125. Epub 2015 Nov 2. PMID: 26707825; PMCID: PMC4915568.
- Isse HM, Lukande R, Sereke SG, Odubu FJ, Nassanga R, Bugeza S. Correlation of the ultrasound thyroid imaging reporting and data system with cytology findings among patients in Uganda. Thyroid Res. 2023 Sep 1;16(1):26. doi: 10.1186/s13044-023-00169-1. PMID: 37653537; PMCID: PMC10472606.
