Vitamin D plays a crucial role in maintaining overall health. The body needs this nutrient for strong bones, proper immune function, and the regulation of various organs. Recent research has explored the relationship between vitamin D and thyroid disorders, particularly hyperthyroidism. This article examines how vitamin D affects thyroid function and what this means for people with an overactive thyroid.
What Is Vitamin D?
Vitamin D is a fat-soluble nutrient that the body produces when skin is exposed to sunlight. Unlike other vitamins that must come from food, the body can manufacture vitamin D naturally. However, people can also obtain vitamin D through dietary supplements and certain foods.
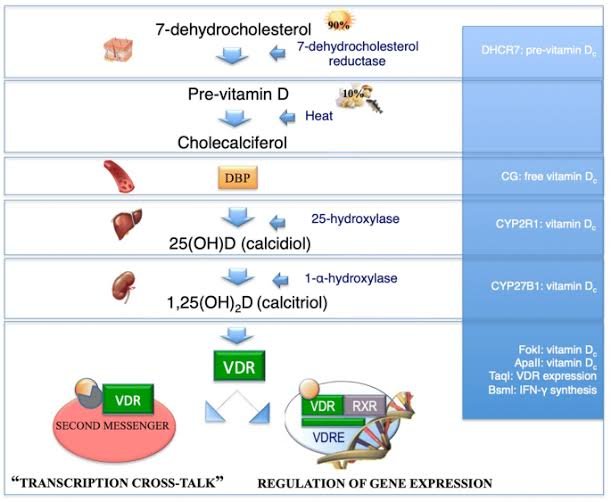
The body must convert vitamin D through several chemical processes before it becomes usable. The final active form is called calcitriol. This activated vitamin D acts as a hormone that regulates many bodily functions.
Vitamin D performs several essential tasks in the body. It helps the body absorb calcium and phosphorus, which are necessary for bone health. Without adequate vitamin D, bones become weak and brittle. Beyond bone health, vitamin D supports immune system function, muscle strength, cardiovascular health, and brain development. Research suggests it may also have anti-cancer properties.
Understanding Hyperthyroidism
Hyperthyroidism occurs when the thyroid gland produces excessive amounts of thyroid hormones. The thyroid is a butterfly-shaped gland located in the neck. It produces hormones that regulate metabolism, energy levels, and body temperature.
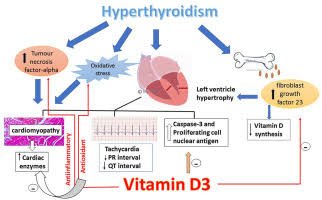
When the thyroid becomes overactive, it releases too much thyroid hormone into the bloodstream. This condition speeds up many bodily processes. Common symptoms include rapid heartbeat, weight loss, increased appetite, nervousness, trembling hands, excessive sweating, and difficulty sleeping.
The most common cause of hyperthyroidism is Graves’ disease, an autoimmune condition. In Graves’ disease, the immune system produces antibodies that stimulate the thyroid gland to produce excess hormones. Other causes include toxic nodular goiter, thyroiditis, and excessive iodine intake.
The Link Between Vitamin D and Thyroid Function
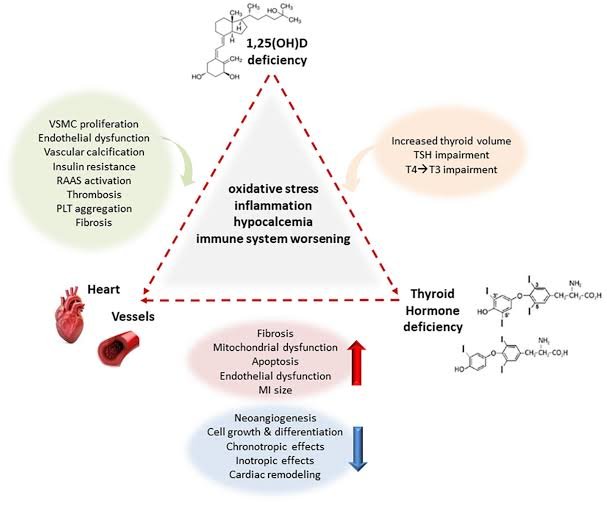
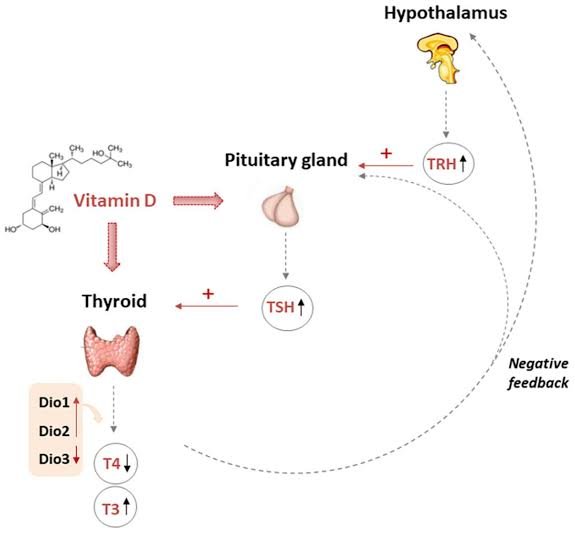
Scientists have discovered important connections between vitamin D levels and thyroid health. The thyroid gland contains vitamin D receptors, which suggests that vitamin D directly influences thyroid function. Research has explored how vitamin D deficiency might affect thyroid conditions.
Studies show that many people with hyperthyroidism have lower vitamin D levels compared to healthy individuals. However, researchers are still determining whether low vitamin D causes thyroid problems or results from them. The relationship appears complex and may work in both directions.
People with Graves’ disease often show particularly low vitamin D levels. This observation has led researchers to investigate whether vitamin D deficiency contributes to the development of autoimmune thyroid diseases. The immune system requires adequate vitamin D to function properly. When vitamin D levels drop too low, the immune system may malfunction and attack the thyroid gland.
How Hyperthyroidism Affects Vitamin D Levels
Hyperthyroidism itself may contribute to vitamin D deficiency through several mechanisms. An overactive thyroid speeds up the body’s metabolism, which includes the breakdown of vitamin D. People with hyperthyroidism may process vitamin D more quickly, converting it into inactive compounds faster than normal. This increased breakdown can deplete vitamin D stores even when intake is adequate.
The symptoms of hyperthyroidism can also indirectly affect vitamin D status. People with an overactive thyroid often experience fatigue, muscle weakness, and anxiety. These symptoms may reduce outdoor activities and sun exposure, limiting the body’s ability to produce vitamin D naturally. Managing thyroid conditions during pregnancy becomes particularly important, as both vitamin D and thyroid hormones are essential for fetal development.
Additionally, hyperthyroidism can affect bone health. The excess thyroid hormone increases bone turnover, leading to bone loss. Since vitamin D is crucial for calcium absorption and bone maintenance, the combination of hyperthyroidism and low vitamin D can significantly compromise bone strength.
Research on Vitamin D and Autoimmune Thyroid Disease
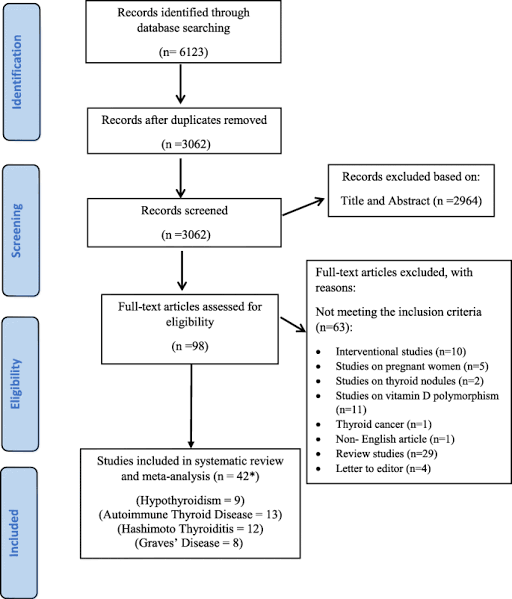
Multiple studies have examined the relationship between vitamin D and autoimmune thyroid conditions like Graves’ disease. A comprehensive review of vitamin D and thyroid function reveals mixed results, but several patterns emerge.
Many observational studies have found an inverse relationship between vitamin D levels and anti-thyroid antibodies. This means that as vitamin D levels decrease, antibody levels tend to increase. Anti-thyroid antibodies are markers of autoimmune activity against the thyroid gland. High levels of these antibodies indicate more severe autoimmune response.
However, not all studies confirm this association. Some research has found no significant connection between vitamin D levels and antibody presence. These inconsistencies may result from differences in study design, participant characteristics, or measurement methods.
Geographic location appears to play a role in vitamin D status and thyroid disease prevalence. Populations living at higher latitudes, where sun exposure is limited, show higher rates of both vitamin D deficiency and autoimmune thyroid disorders. This pattern suggests a possible causal link, though other factors may also contribute.
Vitamin D Supplementation and Thyroid Function
Research on vitamin D supplementation provides encouraging results for people with hyperthyroidism. Multiple studies have tested whether taking vitamin D supplements can improve thyroid function or reduce disease activity.
The most consistent finding is that vitamin D supplementation reduces anti-thyroid antibody levels. Studies have shown that people with Graves’ disease who take vitamin D supplements experience decreases in thyroid-stimulating immunoglobulin (TSI) and thyroid peroxidase antibodies (TPO). These antibodies drive the autoimmune attack on the thyroid gland, so reducing them may help control disease activity.
A recent study on vitamin D supplementation and thyroid health found that participants who received vitamin D supplements showed improvements in thyroid hormone levels and reduced symptoms. The benefits were most pronounced in people who started with severe vitamin D deficiency.
However, vitamin D supplementation does not cure hyperthyroidism. It should be viewed as a complementary therapy that supports conventional treatment rather than a replacement for standard care. People with hyperthyroidism typically require medications to control thyroid hormone production, and some may need radioactive iodine therapy or surgery.
Recommended Vitamin D Levels and Dosing
Health organizations recommend specific vitamin D levels for optimal health. Blood tests measure vitamin D status by checking calcidiol, also called 25-hydroxyvitamin D [25(OH)D]. This form represents vitamin D storage in the body.
Most experts consider vitamin D levels below 20 ng/mL (50 nmol/L) as deficient. Levels between 20-30 ng/mL (50-75 nmol/L) are considered insufficient. Optimal levels range from 30-50 ng/mL (75-125 nmol/L). Some researchers advocate for even higher targets, especially for people with autoimmune conditions.
For general health maintenance, adults should consider taking 400-1000 IU (10-25 mcg) of vitamin D daily. People with documented deficiency may need higher therapeutic doses, sometimes 2000-5000 IU daily or more, under medical supervision. Understanding how to cure thyroid conditions involves addressing multiple factors, including vitamin D status.
The time required to correct vitamin D deficiency varies depending on the severity of deficiency and the dose used. Most people see improvements in vitamin D levels within 2-3 months of starting supplementation. However, it may take longer to observe changes in thyroid function or antibody levels.
Factors That Affect Vitamin D Status
Several factors influence vitamin D levels in the body. Understanding these factors helps people optimize their vitamin D status.
Sun exposure is the primary source of vitamin D for most people. The skin produces vitamin D when exposed to ultraviolet B (UVB) radiation from sunlight. However, many factors affect how much vitamin D the skin can produce. These include skin color, age, geographic location, season, time of day, and sunscreen use.
People with darker skin require longer sun exposure to produce the same amount of vitamin D as those with lighter skin. This is because melanin, the pigment that gives skin its color, reduces vitamin D production. As people age, the skin becomes less efficient at producing vitamin D, even with adequate sun exposure.
Geographic location significantly impacts vitamin D production. People living far from the equator, above 35 degrees latitude, have limited UVB exposure during winter months. During this time, the skin cannot produce sufficient vitamin D regardless of sun exposure duration.
Dietary sources provide some vitamin D, though few foods naturally contain significant amounts. Fatty fish like salmon, mackerel, and sardines are the best dietary sources. Egg yolks, beef liver, and fortified foods like milk and cereals also contribute vitamin D. However, most people cannot obtain adequate vitamin D from diet alone.
Body weight affects vitamin D levels because vitamin D is fat-soluble and gets stored in adipose tissue. People with higher body mass index (BMI) may have lower circulating vitamin D levels because more vitamin D is sequestered in fat tissue. This factor is particularly relevant for people with thyroid disorders, as thyroid function affects metabolism and weight regulation.
Testing and Monitoring Vitamin D Levels
People with hyperthyroidism should consider having their vitamin D levels checked. A simple blood test measures 25(OH)D concentration. Doctors can order this test along with routine thyroid function tests.
The optimal timing for vitamin D testing varies. Some experts recommend testing in late winter or early spring when levels are typically lowest. Others suggest testing before starting supplementation and then rechecking after 2-3 months to assess response.
People with active hyperthyroidism should have their thyroid function monitored regularly regardless of vitamin D status. Standard thyroid tests measure thyroid-stimulating hormone (TSH), free thyroxine (T4), and free triiodothyronine (T3). For those with Graves’ disease, doctors may also check antibody levels.
Monitoring both vitamin D and thyroid function together provides a more complete picture of health status. Changes in one may affect the other, so tracking both helps doctors make informed treatment decisions.
Safety Considerations for Vitamin D Supplementation
Vitamin D supplementation is generally safe when taken at recommended doses. However, excessive intake can cause problems. Vitamin D toxicity, though rare, can occur with very high doses taken over extended periods.
Symptoms of vitamin D toxicity include nausea, vomiting, weakness, and confusion. Severe toxicity can lead to kidney damage and abnormally high calcium levels in the blood. These problems typically only occur with doses exceeding 10,000 IU daily taken for months.
People taking certain medications should use caution with vitamin D supplements. These medications include some diuretics, corticosteroids, and medications for weight loss. Vitamin D can also interact with medications used to treat hyperthyroidism, though significant interactions are uncommon.
Before starting high-dose vitamin D supplementation, people should consult their healthcare provider. This is especially important for those with kidney disease, hyperparathyroidism, sarcoidosis, or a history of kidney stones. These conditions can affect how the body handles vitamin D and calcium.
Vitamin D and Other Thyroid-Related Issues
Vitamin D affects various aspects of health that are particularly relevant for people with thyroid disorders. For example, thyroid conditions often cause hair loss and other scalp problems. While vitamin D alone may not prevent thyroid-related hair loss, maintaining adequate levels supports overall hair health.
Some people with hyperthyroidism develop other health issues that may benefit from vitamin D supplementation. Research indicates that vitamin D supports cardiovascular health, which is important since hyperthyroidism can strain the heart. Adequate vitamin D may help protect against some cardiovascular complications of hyperthyroidism.
Bone health deserves special attention in people with hyperthyroidism. The combination of excess thyroid hormone and low vitamin D creates a particularly high risk for osteoporosis. Studies show that people with hyperthyroidism lose bone density faster than healthy individuals. Ensuring adequate vitamin D intake, along with calcium supplementation, helps protect bone strength.
Diet and Lifestyle Strategies
Beyond supplementation, people can take practical steps to optimize vitamin D status. Regular sun exposure provides natural vitamin D production. Spending 10-15 minutes in midday sun several times per week can significantly boost vitamin D levels. The face, arms, and legs should be exposed without sunscreen during this brief period.
After this short sun exposure, people should apply sunscreen to prevent skin damage. The key is finding a balance between getting enough sun for vitamin D production and protecting skin from excessive UV exposure that increases skin cancer risk.
Dietary choices also matter. Including vitamin D-rich foods in the diet supports overall nutrient status. Following a hypothyroidism diet plan that includes vitamin D-rich foods benefits people with various thyroid conditions. While dietary vitamin D alone is usually insufficient, it complements sun exposure and supplementation.
Regular physical activity supports bone health and may help improve vitamin D metabolism. Exercise also benefits people with hyperthyroidism by reducing anxiety and promoting better sleep. Activities like walking, swimming, and gentle strength training are particularly beneficial.
The Role of Vitamin D in Immune Function
Understanding vitamin D’s role in immune function helps explain its connection to autoimmune thyroid disease. Vitamin D modulates both the innate and adaptive immune systems. It helps regulate the production and activity of immune cells.
When vitamin D levels are adequate, the immune system functions more effectively at fighting infections while avoiding attacks on the body’s own tissues. Low vitamin D levels may allow the immune system to become dysregulated, increasing the risk of autoimmune reactions.
Research shows that vitamin D influences T cells, which are crucial components of the immune system. These cells help determine whether the immune system responds appropriately to threats or mistakenly attacks healthy tissue. In Graves’ disease, T cells incorrectly target the thyroid gland. Adequate vitamin D may help prevent or reduce this inappropriate immune response.
Vitamin D also affects the production of inflammatory molecules called cytokines. Some cytokines promote inflammation, while others reduce it. Vitamin D generally shifts the balance toward less inflammation, which may benefit people with autoimmune conditions like Graves’ disease.
Current Research and Future Directions
Scientists continue investigating the relationship between vitamin D and thyroid function. Recent research explores new aspects of this connection and refines our understanding of how vitamin D supplementation might benefit people with thyroid disorders.
Current studies are examining several key questions. Researchers want to determine the optimal vitamin D dose for people with hyperthyroidism. They are also investigating whether vitamin D supplementation can prevent the development of thyroid disease in high-risk individuals. Additionally, scientists are studying whether vitamin D can reduce the need for conventional thyroid medications or improve treatment outcomes.
Some studies are exploring the genetic factors that influence how individuals respond to vitamin D. Variations in genes related to vitamin D metabolism and vitamin D receptors may explain why some people benefit more from supplementation than others. This personalized approach could lead to more targeted vitamin D recommendations.
Future research will likely involve larger clinical trials with longer follow-up periods. These studies will help clarify whether vitamin D supplementation should become a standard part of hyperthyroidism treatment. They will also identify which patients are most likely to benefit from supplementation.
Practical Recommendations for People with Hyperthyroidism
People with hyperthyroidism should take several practical steps regarding vitamin D. First, ask your doctor to check your vitamin D level. This baseline measurement helps determine whether supplementation is needed and at what dose.
If vitamin D levels are low, start supplementation as recommended by your healthcare provider. Most people benefit from taking vitamin D3 (cholecalciferol), which is more effective than vitamin D2 (ergocalciferol) at raising blood levels. Take vitamin D supplements with food, especially meals containing some fat, as this improves absorption.
Continue taking prescribed thyroid medications as directed. Vitamin D supplementation supports but does not replace conventional treatment for hyperthyroidism. Regular follow-up with your doctor ensures that both thyroid function and vitamin D levels are monitored appropriately.
Make lifestyle changes that support vitamin D production and overall health. Get regular sun exposure when possible, eat a balanced diet that includes vitamin D-rich foods, exercise regularly, and maintain a healthy weight. These strategies work together to improve both vitamin D status and thyroid health.
Pay attention to bone health, which is particularly important for people with hyperthyroidism. Ensure adequate calcium intake along with vitamin D. Consider having a bone density scan if you have had hyperthyroidism for an extended period or are at high risk for osteoporosis.
Conclusion
The relationship between vitamin D and hyperthyroidism is complex but important. Evidence suggests that people with hyperthyroidism often have low vitamin D levels. This deficiency may contribute to disease development or severity, particularly in autoimmune conditions like Graves’ disease.
Vitamin D supplementation shows promise as a complementary therapy for hyperthyroidism. Studies consistently show that supplementation reduces anti-thyroid antibody levels and may improve symptoms. However, vitamin D is not a cure for hyperthyroidism and should be used alongside conventional medical treatment.
People with hyperthyroidism should have their vitamin D levels checked and consider supplementation if levels are low. The combination of adequate vitamin D, proper medical treatment, and healthy lifestyle choices offers the best approach to managing hyperthyroidism and protecting long-term health.
While research continues to clarify the exact mechanisms and optimal treatment strategies, current evidence supports maintaining adequate vitamin D levels as part of comprehensive thyroid care. Talk to your healthcare provider about testing and supplementation to determine the best approach for your individual situation.